Treatments for Reflux or GERD
Treatments for Reflux or GERD Main Content
Treatments for Reflux or GERD
Do you struggle with persistent heartburn? Do your reflux symptoms keep you up at night? Have you been using antacids every day for more than two weeks? If so, our team at Baptist Health is here to help you.
What is the difference between Acid Reflux and GERD?
While acid reflux is a medical condition that ranges from mild to severe, GERD (gastroesophageal reflux disease) is a chronic, more serious form of acid reflux. Common symptoms of GERD may include:
- Frequent heartburn
- Regurgitation
- Dry cough
- Sore throat
- Asthma symptoms
- Trouble swallowing
- Trouble staying asleep
Symptoms of GERD should not be managed by suffering through, or waiting it out. Chronic acid reflux causes more than acute discomfort; it can cause long-term damage and even cancer if left untreated.
Content Section 1
How can we help you?
It looks like there was a problem
Try going back and resubmitting the form.
Thank you for submitting your request
We appreciate you taking the time to reach out to us. Our team is currently reviewing your submission and will be in touch shortly with the next steps. We look forward to assisting you soon!
Content Section 2
Meet the Surgeons
Surgeons providing care at Baptist Medical Center Jacksonville, Baptist Beaches and Baptist Nassau can help you determine the best solution for your reflux symptoms.
Baptist Jacksonville:
-
Craig Morgenthal, MD, FACS
General Surgeon
-
Steven Hodgett, MD, FACS
General Surgeon
Baptist Jacksonville and Baptist Nassau:
-
Mark Diebel, MD
General Surgeon
Baptist Beaches:
-
Brian Dalton, MD
General Surgeon
Content Section 3
Diagnosing GERD
Of course, some routine testing is needed before a final decision about treatment can be made. Standard diagnostic screenings typically include:
-
Upper Endoscopy (EGD)
Using an endoscope (a long, flexible tube with a small light and camera at the end), doctors look down your mouth, throat, esophagus, stomach, and into your duodenum.
-
Esophageal pH Test (48-hour Bravo)
By placing a pH capsule to the wall of your esophagus, this test monitors whether acid is coming back into the esophagus.
-
Video Esophagram (VEG) for Dysmotility
A barium swallow test, followed by a swallow of a piece of a bagel, followed by a swallow of a piece of marshmallow.
-
High Resolution Manometry (HRM)
To measure the pressure in your esophagus a thin, small computerized tube, after you are numbed, is placed from your nose to your lower-esophageal sphincter while 10 swallows of water are evaluated in a resting position.
Content Section 4
Treatment Options for GERD
-
Lifestyle Changes and Medication
Treatments typically start with lifestyle and dietary changes to relieve symptoms of reflux. Millions of people with GERD use over-the-counter medications or take prescription medications (such as H2 blockers, or PPI - proton pump inhibitors).
However, taking medications long term can have dangerous side effects and is not recommended.
-
Minimally-Invasive Procedures
If changing your diet or habits doesn’t help and you rely on medications to manage your symptoms, it may be time to consider another solution. Our team at Baptist Health specializes in minimally invasive procedures to give you long-term relief from reflux symptoms and help prevent more serious health issues.
Using laparoscopic and robotic techniques, patients typically spend one night in the hospital for recovery.
-
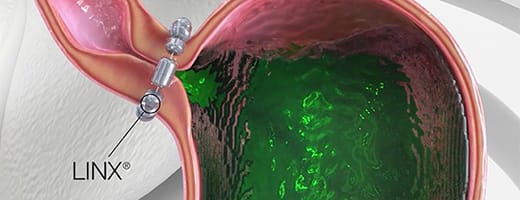
LINX Reflux Management System
The LINX© Reflux Management System is a small, flexible band of magnets enclosed in titanium beads. The system is implanted around the lower esophageal sphincter (LES), just above the stomach. The magnetic beads keep the esophageal sphincter closed to help prevent reflux. The beads temporarily separate to allow food and liquid to pass into the stomach.
-
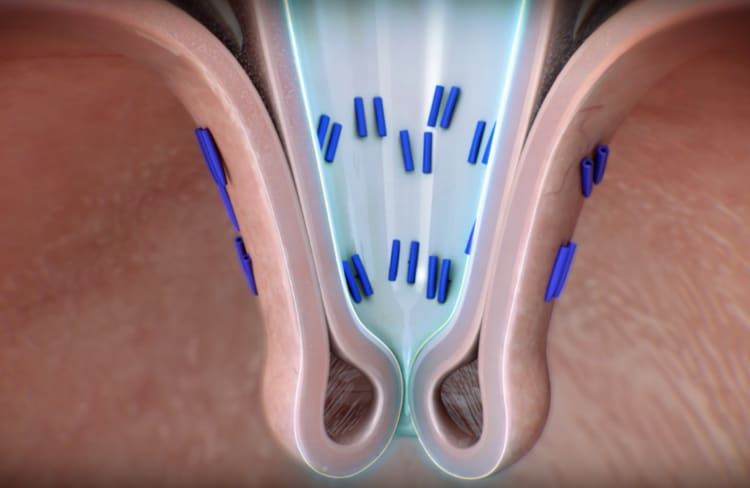
TIF Procedure
Transoral lncisionless Fundoplication (TIF) is an incisionless procedure that treats GERD by reconstructing the anti-reflux valve. Going through the mouth, there are no scars, minimizing complications and possibly leading to a quicker recovery.
-

Fundoplication Procedures
Fundoplication is a minimally-invasive surgical technique that reinforces the lower esophageal sphincter by wrapping part of the stomach around the bottom of the esophagus. Fundoplication is often done laparoscopically, which only involves small incisions in the abdomen. The surgeons are trained in both laparoscopic Nissen and Toupet fundoplication techniques.
-
For Obese Patients: Gastric Bypass
For patients who are morbidly obese, the best anti-reflux procedure is usually gastric bypass. Gastric bypass surgery treats GERD by creating a smaller stomach pouch and rerouting the digestive tract. This reduces stomach acid and food flow back into the esophagus, relieving GERD symptoms. In addition to reflux control, gastric bypass also allows successful weight loss and improvement in medical issues.
Content Section 5
Patient Stories
-

Oh my GERD
Living with acid reflux doesn’t have to be your normal.
Physicians providing care at our hospitals are not employees or agents of the hospital.